Kalamunda Hospital Safety and Quality
Our goal is to provide our patients with the highest possible quality care. This is regularly measured by feedback provided through a range of methods, including patient feedback, in addition to the measurement of expected outcomes against patient safety targets.
Through programs of surveillance, audit and inquiry, we empower our staff to continually improve the quality of care provided and to strive towards the provision of amazing care – in line with our organisation’s key objective.
Our aim is always to provide people suffering from a medical condition with best-practice care and treatment while in hospital. However, sometimes in spite of the best care, other health or medical problems arise - either related to the primary diagnosis or related to care or treatment. This is referred to as a complication. A hospital-acquired complication (HAC) is a complication for which clinical risk mitigation strategies may reduce, but not necessarily eliminate, the likelihood of that complication occurring.
The national list of 16 HAC Groups was developed by the Australian Commission on Safety and Quality in Health Care through a comprehensive process that included reviews of the literature, clinical engagement and testing of the concept with public and private hospitals. The HACs list identifies agreed types of high-priority complications that clinicians, managers and others can work together to address and improve patient care.
The 16 HAC groups are:
- Pressure Injury
- Falls resulting in fracture or other intracranial injury
- Healthcare associated infection
- Surgical complications requiring unplanned return to theatre
- Unplanned intensive care unit admission
- Respiratory complications
- Venous thromboembolism
- Renal failure
- Gastrointestinal bleeding
- Medication complications
- Delirium
- Persistent incontinence
- Malnutrition
- Cardiac complications
- Third and fourth degree perineal laceration during delivery
- Neonatal birth trauma
Measuring hospital-acquired complication rates
Primary and secondary diagnoses and complications are routinely recorded for every admission in administrative databases after discharge. Analysis of this “coded data” provides health services with information about the occurrence of complications.
If one or more complications from the HAC Groups occurs during an admission, then that admission is counted as “an admission with one or more HAC” or “HAC Episode”. Sometimes there may be more than one complication from the same HAC Group, or complications from two or more different HAC groups.
The chart that follows shows HAC Episodes (Groups 1-14 only) for Kalamunda Hospital combined as a percentage of all admissions per year since 2018.
How do we measure up
The graph below shows the percentage of admissions for Kalamunda Hospital.
Chart: Percentage of admissions with one or more hospital acquired complications.
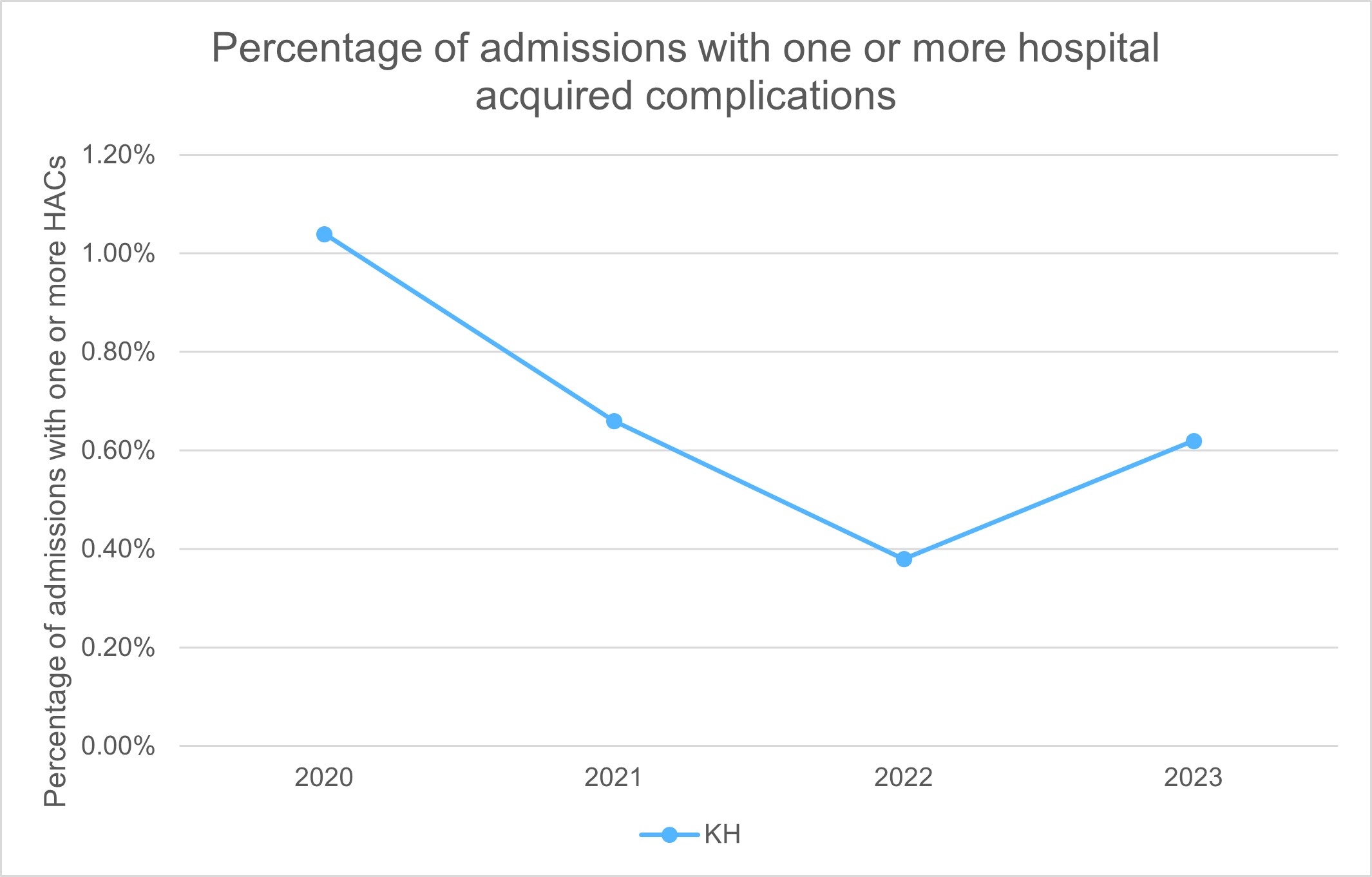
What the figures mean
A lower percentage indicates fewer complications and is desirable. Although no benchmark has been set for this indicator, KH constantly strives to reduce the number of hospital acquired complications through a broad range of improvement initiatives.
Each year nearly one quarter of people over 60 years of age will experience a fall. For some people, the injuries caused by their fall may be so serious that they can no longer live independently.
Falls account for over 80 per cent of all injury-related hospital admissions for people aged 65 years and older. They can occur at any age, but the frequency and severity of falls-related injuries increases significantly with age and frailty.
Unfortunately, falls are one of the most frequently reported clinical incidents in hospitals worldwide and it is known that there is a correlation with:
- length of hospital stay
- care and use of health resources
- discharge rates to a nursing home or residential care facility.
Measuring hospital-acquired complications – Falls
The World Health Organization (WHO) defines a fall as an event which results in a person coming to rest accidentally on the ground, floor or other lower level. This definition covers all types of falls-related clinical incidents, including:
- near-misses
- intercepted falls where the patient is lowered to the ground
- suspected/unwitnessed slips/trips/falls
- witnessed slips/trips/falls.
Fall-related injury is one of the leading causes of hospital-acquired morbidity and mortality in older Australians, and typically leads to pain, bruising and lacerations and fractures. Falls can also lead to intracranial bleeding, which can cause confusion, drowsiness, clouding, loss of consciousness and headache.
Healthcare commonly uses rates to measure complications such as these. The number of patients who have a fall in hospital resulting in fracture or intracranial injury per 1,000 patient days.
How do we measure up
The graph below shows the combined rate of reported falls incidents for Kalamunda Hospital.
Chart: Rate of falls in hospital resulting in fracture or intracranial injury.
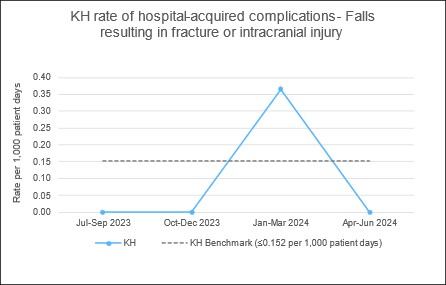
What the figures mean
The benchmark is less than or equal to 0.152 falls in hospital resulting in fracture or intracranial injury per 1,000 patient days. A rate lower than the benchmark is desirable.
Kalamunda Hospital results have been below the benchmark in three quarters out of the last four quarters. Kalamunda Hospital constantly strives to reduce the rate of falls incidents and preventative strategies continue to be put in place.
A pressure injury is a sore, break or blister of the skin caused by unrelieved pressure or friction on an area of the body over a period of time. The depth of skin damage can vary from shallow to very deep. Pressure injuries can be very painful and take a long time to heal. They may also reduce a patient’s mobility.
Older people are at most risk of pressure injuries, but they can occur in any patient or in any setting, including:
- acute areas such as operating theatres
- during transportation to a hospital
- intensive care units.
The majority of pressure injuries are preventable; however those at greater risk include the frail, elderly or people who have:
- been confined to a bed or chair
- poor bladder or bowel control
- diabetes, poor circulation or a history of smoking
- reduced mental awareness due to illness, medications or anaesthetics
- poor diet or fluid intake.
Pressure injuries may impact significantly on a patient’s:
- length of hospital stay
- comfort and quality of life
- cost of care and health outcomes.
Measuring hospital-acquired complications – Pressure injury
The international pressure injury classification systems provide a consistent and accurate means to communicate and document the severity of a pressure injury between clinical staff. The classification system grades these types of wounds in stages depending on:
- changes in the patient’s skin
- the depth of the injury
- whether there is any fluid draining from the wound.
Healthcare commonly uses rates to measure complications such as these. The number of patients who developed one or more Stage 3 or greater pressure injuries during their hospital stay per 1,000 patient days.
How do we measure up
The graph below shows the combined inpatient pressure injury rate for Kalamunda Hospital.
Chart: Rate of hospital-acquired pressure injuries.
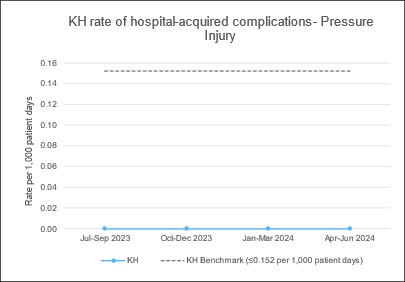
What the figures mean
The benchmark is less than or equal to 0.152 hospital-acquired pressure injury per 1,000 patient days. A rate lower than the benchmark is desirable.
Kalamunda Hospital results have been better than the benchmark in all of the last four quarters.
Medicines are the most common treatment used in health care and contribute to significant improvements in health when used appropriately. However, because they are the used in complex healthcare environments – and despite the policies and procedure in place – there has been times when an error or adverse event has occurred.
Medication complications may indicate a failure in the medication management process that leads to, or has the potential to lead to, harm to the patient. Hospital-acquired medication complications prolong the length of hospitalisation, which impacts on patients and their families.
Medication complications can occur when:
- choosing a medicine
- writing the prescription
- preparing or manufacturing the medication
- dispensing the medication
- administering or taking the medication
- monitoring post-administration of the medication to the patient.
Measuring Hospital-acquired complications – Medication complications
Healthcare commonly uses rates to measure complications such as these. The number of patients who had a hospital-acquired medication complication during their hospital stay per 1,000 patient days.
How do we measure up
The graph below shows the combined medication related incidents rate for Kalamunda Hospital.
Chart: Rate of hospital-acquired medication complications.
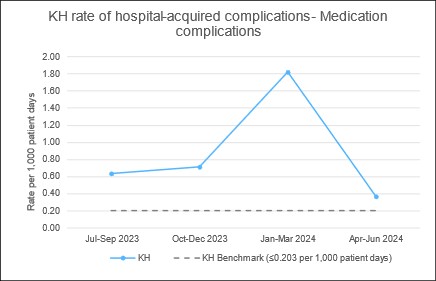
What the figures mean
The benchmark is less than or equal to 0.203 hospital-acquired medication complications per 1,000 patient days. A rate lower than the benchmark is desirable.
The Kalamunda Hospital rate has been consistently above the benchmark. Kalamunda Hospital constantly strives to reduce the rate of medication complication incidents and preventative strategies continue to be put in place.
Infections people get while being cared for in a healthcare facility are known as healthcare associated infections (HAI).
The most common types of infection acquired in hospitals are:
- bloodstream infection
- urinary tract infection (UTI)
- pneumonia (lung infection)
- wound infection.
For a patient, a HAI can result in:
- illness
- an extended stay in hospital
- a slower recovery
- increased stress
- lower morale.
While HAIs are costly to patients, hospitals and the community, financial impact is just one factor which needs to be considered when addressing the issue, with the stress caused to the patient also a key consideration. While they can occur in any healthcare setting, effective infection prevention and control can significantly reduce the infection rate. Patients, visitors and staff all play a role in reducing HAIs.
About Staphylococcus aureus bloodstream infections (SABSIs)
An important cause of common HAI is Staphylococcus aureus (S. aureus), also known as ‘Golden Staph’. It is a type of bacteria often found on the skin of healthy people and is usually harmless. In hospitals, transmission is most commonly via the hands of healthcare workers.
Most cases can be treated by antibiotics; however, there are more serious antibiotic-resistant strains. It is estimated that contracting a healthcare-associated S. aureus bloodstream infection whilst in hospital, can be life-threatening or cause serious harm in 20 to 35 per cent of cases.
Measuring hospital acquired bacteraemia
The rate of healthcare associated S. aureus bloodstream infections (SABSIs) is measured by counting the number of infections and dividing by the number of beds occupied by patients each day (occupied bed days) over a three-month period. For an infection to be considered healthcare-associated there must be no evidence that it was present or developing at the time of hospital admission.
The definition of a SABSI was developed by the Australian Commission on Safety and Quality in Health Care.
The nationally agreed benchmark set under the National Healthcare Agreement (NHA) is no more than 2.0 cases of healthcare associated S. aureus bloodstream infection per 10,000 days of patient care for public hospitals in each state and territory.
WA Health has set a benchmark of less than or equal to 1.0 healthcare associated S. aureus bloodstream infection per 10,000 bed days.
To minimise the risk of patients getting a preventable infection, each EMHS hospital has a surveillance program through which they closely monitor infection rates and evaluate the effectiveness of strategies used to prevent and control SABSIs. Surveillance data is reported throughout all levels of the health service to support good decision-making in the prevention of SABSIs.
All identified cases of infection undergo review by infection control specialists to ascertain anything that the service could have done to prevent the infection. Given the complexity of health care and patients seen, not all cases of infection will be considered preventable.
How do we measure up
The graph below shows the combined healthcare associated bacteraemia rate for Kalamunda Hospital.
Chart: Healthcare-associated S. aureus bloodstream infection rate per 10,000 bed days.
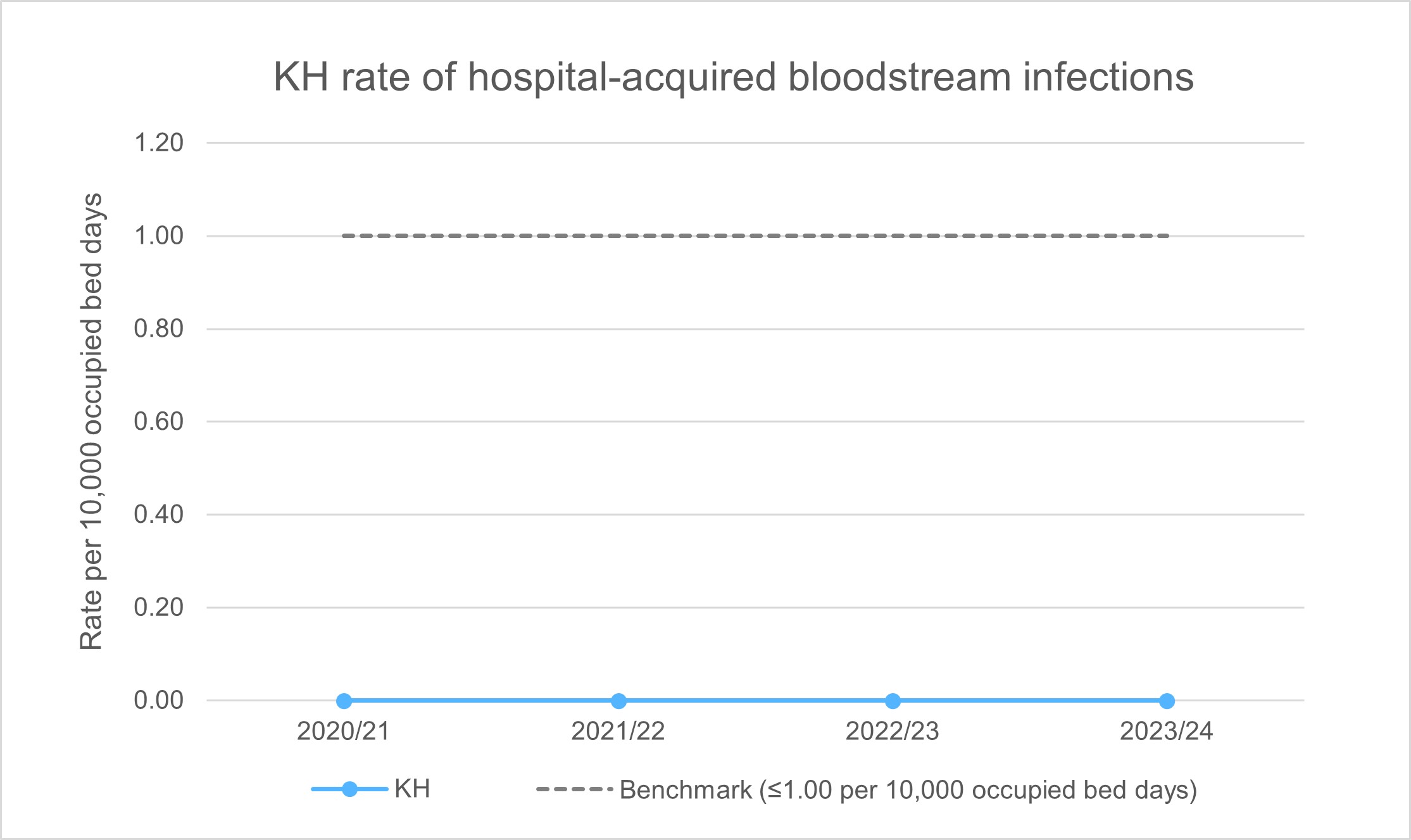
What the figures mean
The graph shows the overall rate of S. aureus bloodstream infection across Kalamunda Hospital by financial year (FY).
The benchmark is less than or equal to 1.0 hospital-acquired bloodstream infection per 10,000 occupied bed days. A rate lower than the benchmark is desirable.
The rate of S. aureus bloodstream infections at Kalamunda Hospital has been consistently below the benchmark. KH continues to monitor, review and identify strategies towards prevention of infection.
Good hand hygiene (washing or decontaminating hands with soap and water or an alcohol-based hand rub) is an important part of good patient care.
Hand Hygiene Australia (HHA) describes improving hand hygiene among healthcare workers as the single most effective intervention in reducing healthcare-associated infections (HAI) in Australian hospitals. The aim is for healthcare workers to perform hand hygiene correctly at every opportunity, for example, before and after touching a patient.
The National Hand Hygiene Initiative (NHHI) was implemented to develop a national approach to improving hand hygiene and monitor its effectiveness. Although not nationally comparable, hand hygiene information helps to drive quality improvement in hospitals.
Measuring hand hygiene compliance
Hand hygiene is measured by observing a specified number of ‘moments’ before and while caring for patients:
- Moment 1: Before touching a patient
- Moment 2: Before a procedure
- Moment 3: After a procedure or body fluid exposure risk
- Moment 4: After touching a patient
- Moment 5: After touching a patient’s surroundings.
The estimated hand hygiene rate for a hospital is a measure of how often hand hygiene is correctly performed (as a percentage). It is calculated by dividing the number of observed hand hygiene ‘moments’ where proper hand hygiene was practiced in a specified audit period, by the total number of observed hand hygiene ‘moments’ in the same audit period and multiplying by 100. The rate is rounded to one decimal place.
Hand hygiene data is provided by State and Territory health services for public hospitals and by individual private hospitals. The data is derived from audits of hand hygiene ‘moments’ conducted up to 3 times per year through the National Hand Hygiene Initiative. Audits are performed by individuals who have undergone HHA auditor training.
The Australian Commission on Safety and Quality in Health Care recommends a benchmark hand hygiene rate of 80 per cent.
How do we measure up
The graph below shows the combined hand hygiene compliance rate for Kalamunda Hospital.
Chart: Kalamunda Hospital hand hygiene results for audit periods.
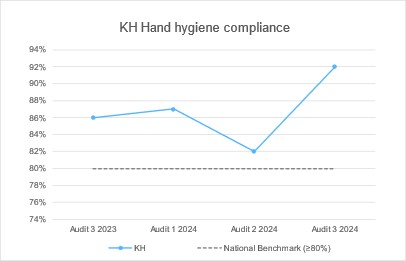
What the figures mean
The graph shows the hand hygiene compliance rate for Kalamunda Hospital for the last four audit periods. A rate higher than the benchmark is desirable.
In the last four audit periods, Kalamunda Hospital has consistently achieved greater than the benchmark of 80% compliance.
Listening to and acting on feedback from our patients, their families and their carers about our health services is one of the most important aspects of delivering high quality care.
Complaints about provision of health care services can be made by anyone who has contact with our services. People who complain often have some basic expectations, they want to:
- be heard and understood
- be respected
- be taken seriously
- be given support or assistance if required
- have their concerns dealt with effectively and efficiently
- be informed of the process, progress, findings and outcome
- have appropriate action taken as a result of their complaint.
Communication issues underpin most complaints we receive, and most people who submit a complaint are simply looking for an explanation or apology. Another common motivation behind complaints is to prevent the same thing happening to others. This is why acknowledging complaints promptly and letting people know what's been done to prevent it happening again is so important.
The complaint management process is not intended to apportion blame but strives to resolve the complaint, if possible, and identify any aspects of service delivery which require change in order to effect improvement.
Measuring complaint numbers and actions taken
The Health and Disability Services Complaints Act 1995 and Regulations 2010 legislate for the annual provision of information relating to complaints received by the health service provider, and action taken, to the Health and Disability Services Complaints Office.
The key issues associated with a complaint about our health service are determined by EMHS staff in discussion with the person making the complaint. Identifying the issues in the complaint provides for effective resolution and allows all parties to have an understanding of the issues raised. Each complaint received must have at least one complaint issue identified, with the possibility for multiple issues to be identified in one complaint. Similarly each complaint will have at least one resolution achieved, with the possibility of multiple resolutions being achieved for one complaint.
Complaints rate
How do we measure up
The graphs below show the combined complaints numbers for Kalamunda Hospital.
Chart 1: Complaints rate per 1,000 bed days.
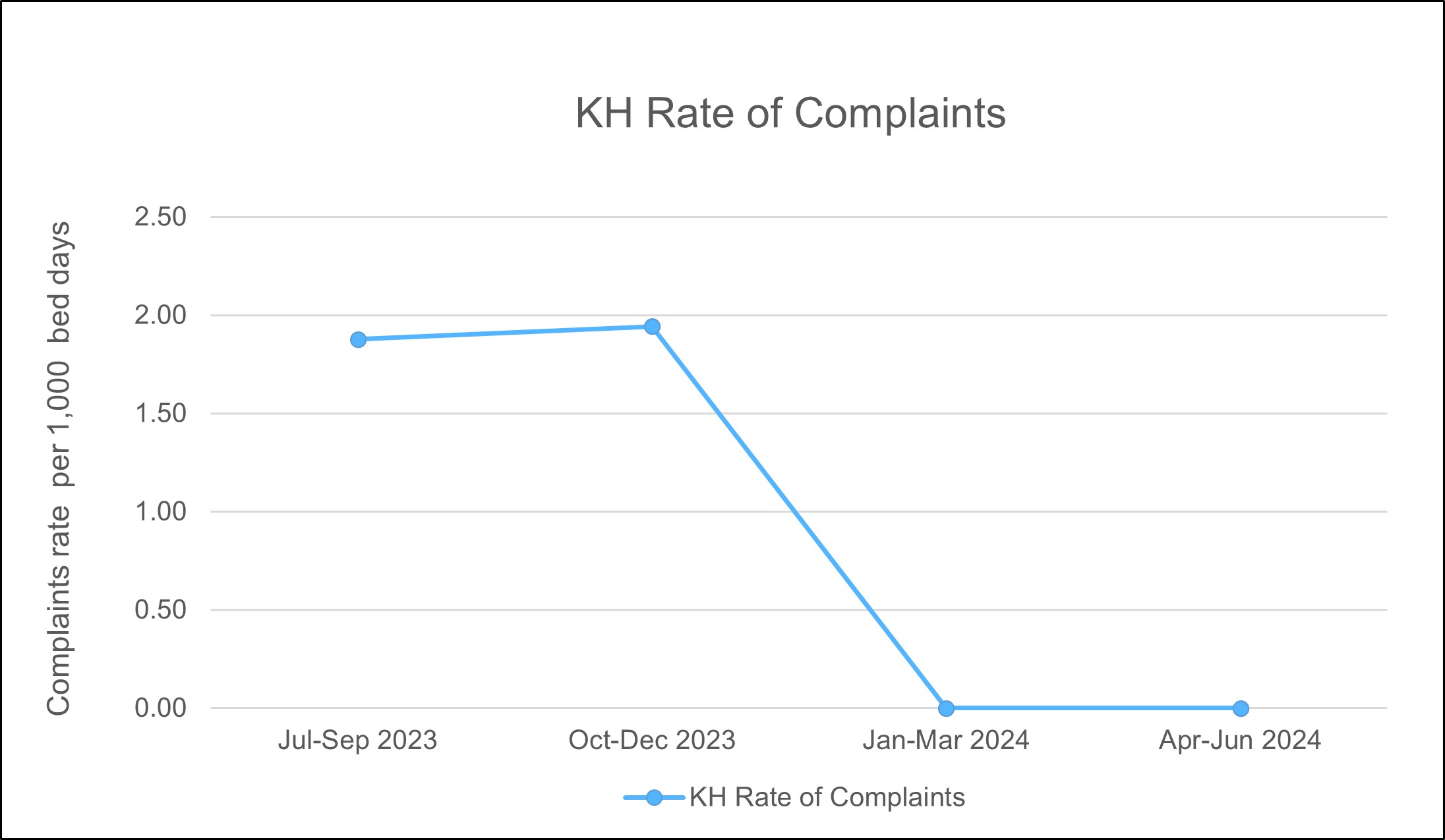
What the figures mean
This graph shows the rate of complaints for Kalamunda Hospital for the period July 2023 to June 2024. Kalamunda Hospital encourages consumers to provide feedback on the care they receive and uses the feedback to continuously learn and improve the services they deliver.
Complaint issues
How do we measure up
The graph below shows the combined top categories of complaint issues for Kalamunda Hospital.
Chart 2: Top categories of complaint issues.
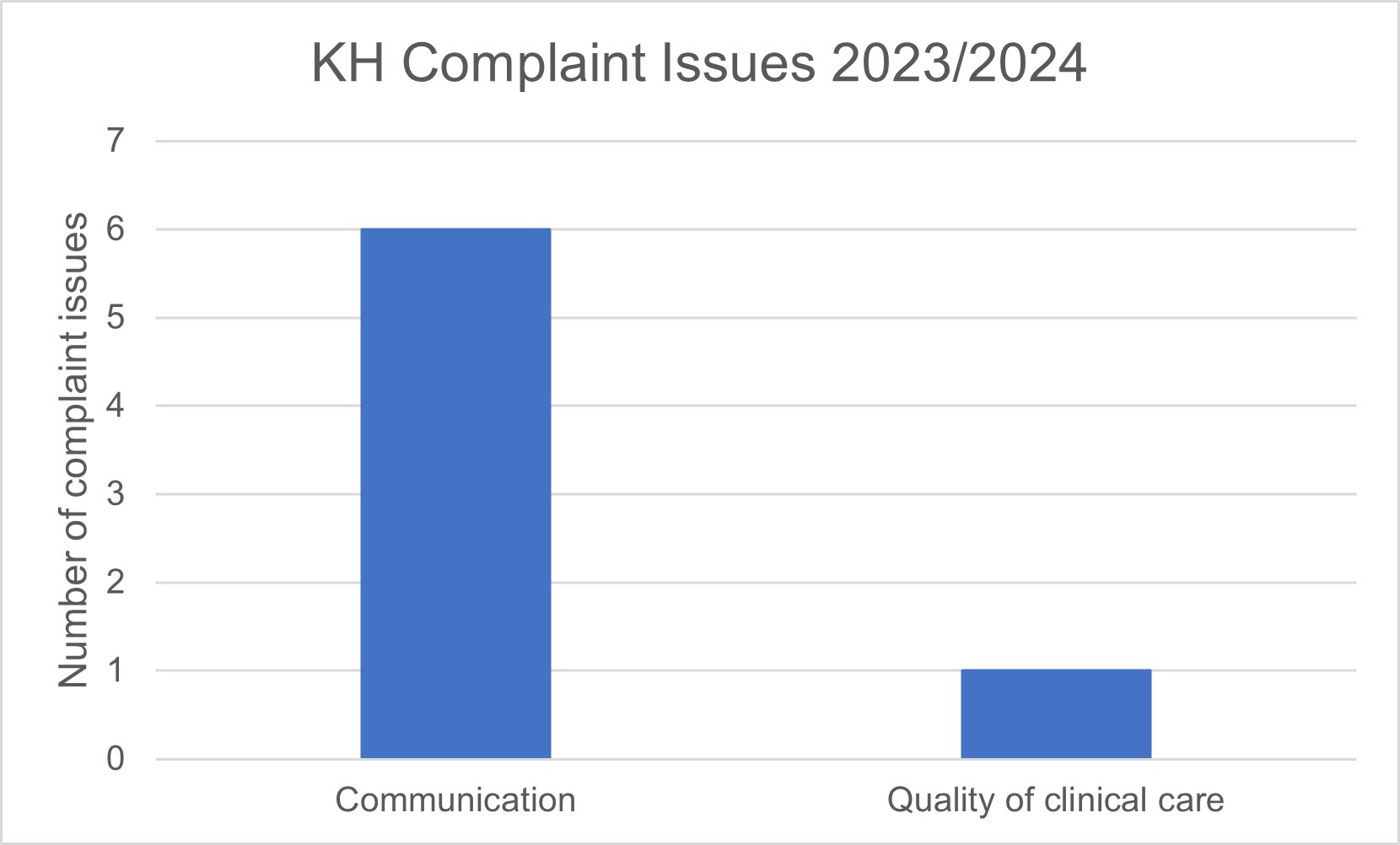
What the figures mean
The most common categories of complaint issues were ‘Communication’ and ‘Quality of clinical care’. Between them, these accounted for 70% of all issues.
Complaint resolutions
How do we measure up
The graph below shows the combined top resolutions to complaints for Kalamunda Hospital.
Chart 3: Top complaint resolutions.
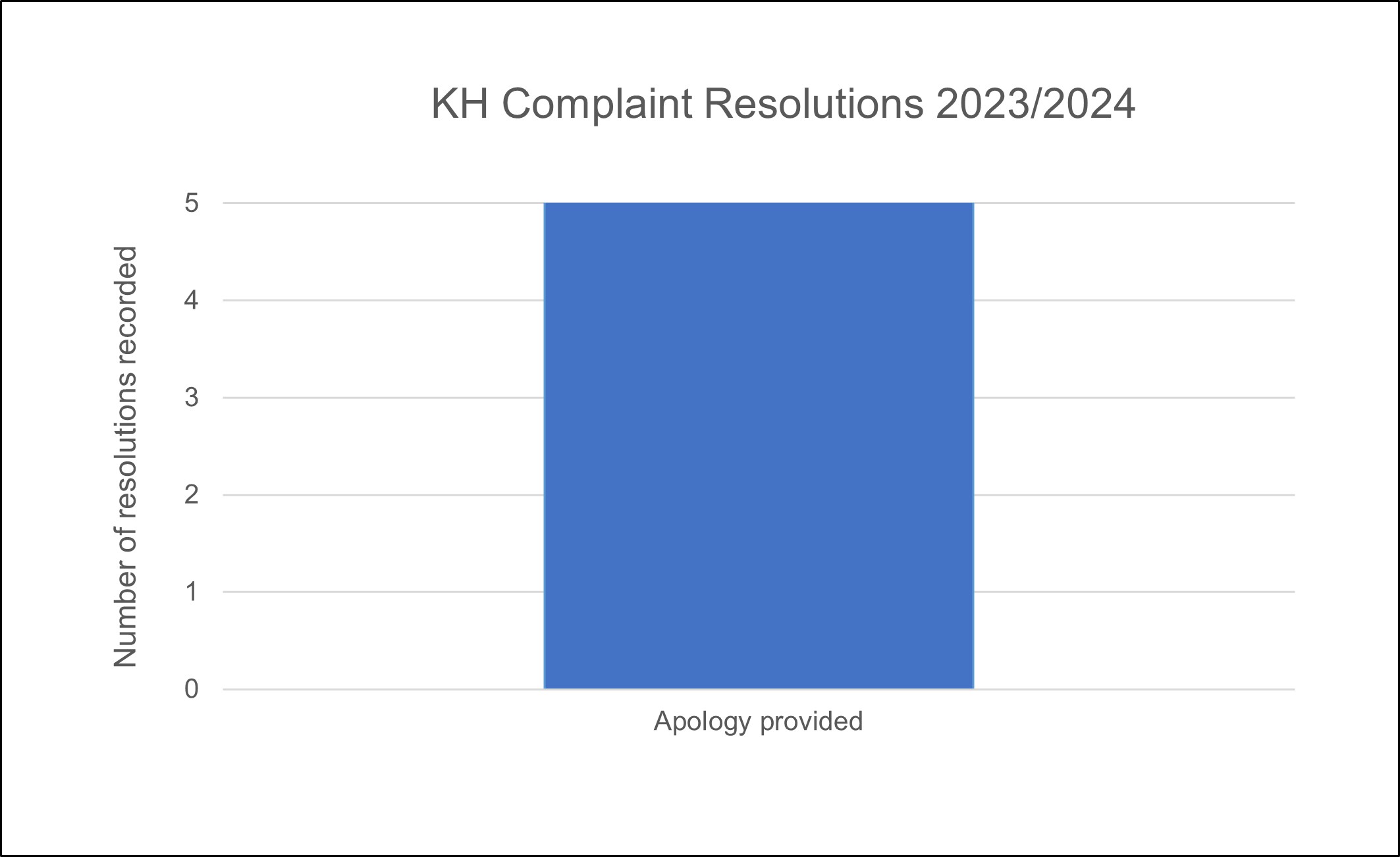
*Note: One complaint may have more than one resolution, so the count of resolutions may be greater than the number of complaints.
What the figures mean
The most common resolution of complaints was Apology provided.
It is an unfortunate reality that no system which delivers complex health care is free from risk or error. It is globally recognised (World Health Organisation, 2017) that errors in healthcare delivery are the cause of unintended harm and at times, associated with poor outcomes for patients.
Ensuring patient safety and the delivery of high quality care at all times is the number one priority for EMHS. To support this, EMHS has a proactive and transparent patient safety culture that uses a non-punitive approach to the reporting of and learning from, clinical incidents or errors.
So that the health service can adequately investigate the causes of clinical incidents, each incident is assigned a rating known as a Severity Assessment Code (SAC) score that guides staff in the type of investigation method to be applied to each event. Clinical incidents that result in serious harm or death (SAC 1) require a very detailed, rigorous investigation facilitated by an expert panel, members of which may at times be completely independent to the health service.
Measuring high level incident overviews and strategies
Clinical incidents can be represented as a rate per 1,000 occupied bed days. This can give an idea of how busy a hospital is at the time that incidents are reported, and can help inform us about how successful the culture of open and transparent reporting is.
When an incident is reported and investigated, one of the things reported is whether a patient is injured and how severe the injury is. We try to learn from every incident, whether or not the incident causes harm, and make changes to systems, processes and procedures to reduce the risk of future incidents happening, and to prevent harm from similar incidents if they do happen. This is the reason that we promote a culture of openness and transparency we prevent future harm If an incident is reported as a near-miss, or causing no harm.
How do we measure up
The graph below shows the combined incident rate for Kalamunda Hospital.
Chart: Rate of reporting of clinical incidents per 1,000 occupied bed days: All reported inpatient clinical incidents and inpatient clinical incidents resulting in harm.
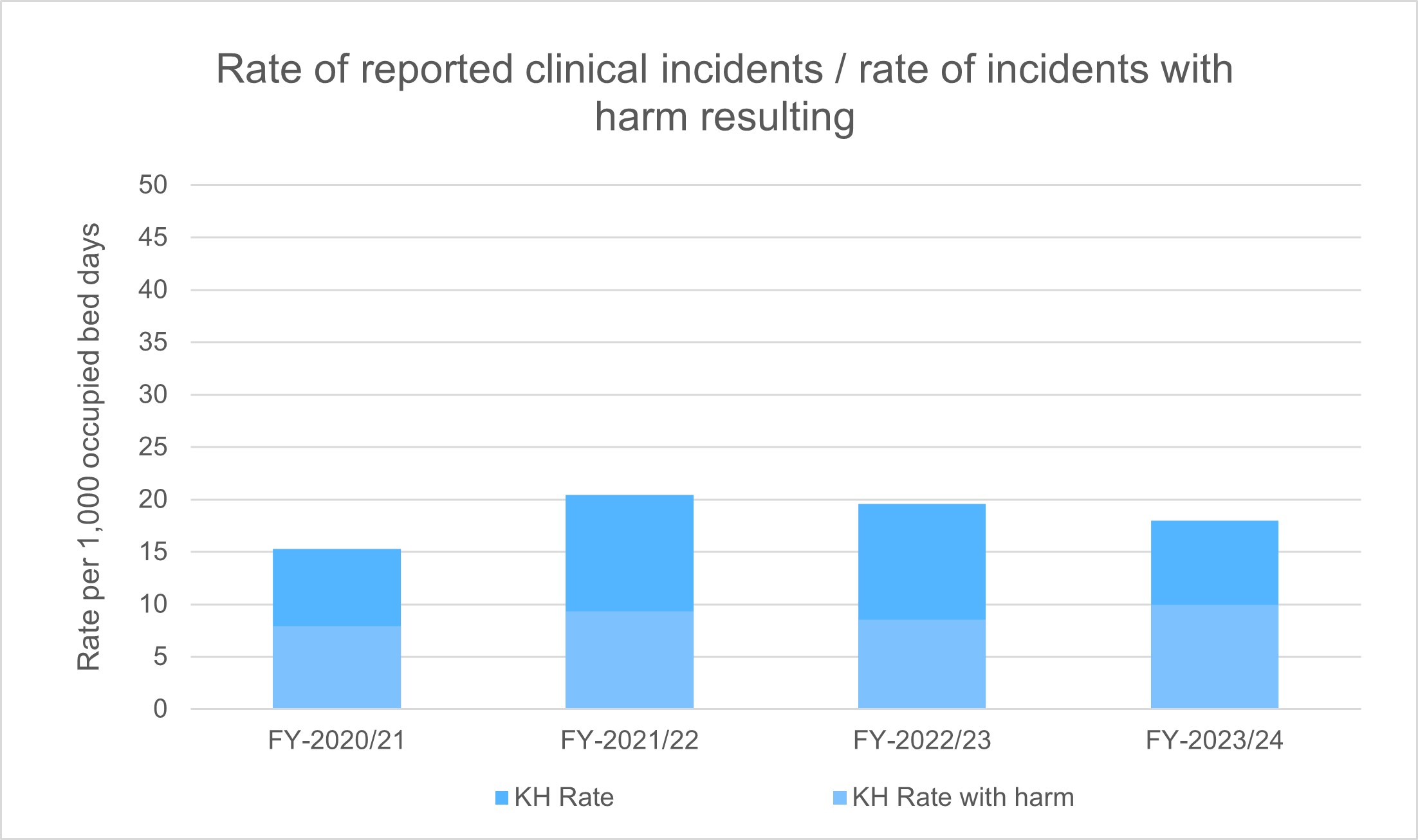
What the figures mean
The graph shows the rate of reported inpatient clinical incidents per 1,000 bed days. The darker coloured bar shows the total rate of all inpatient clinical incidents, and the lighter coloured bar shows the rate and fraction of incidents that resulted in harm of any kind.
The higher total rate of reported incidents and the consistently high rate of reporting show that the culture of reporting incidents is healthy and effective. Note that the rate of incidents resulting in harm has remained low – this shows that the health system learns from events and introduces effective programs to prevent and minimise harm resulting from incidents.
 Receiving and listening to stories from our patients, their families and their carers provide valuable feedback about the quality of the healthcare we provide.
Receiving and listening to stories from our patients, their families and their carers provide valuable feedback about the quality of the healthcare we provide.
Care Opinion is an online platform that enables members of the public to tell us about their experience with our services. This information is used to improve services and to recognise staff and teams who may go above and beyond our patient's expectations.
See what our patients are saying about us and how we are responding (external site).
Measuring Care Opinion
Since Kalamunda Hospital introduced Care Opinion, the hospital has had:
What have people been telling us
Kalamunda Hospital patients are encouraged to tell us about their experience with the hospital.
The most recent stories from our patients are:
What have we done to improve
As a result of what our patients tells us, Kalamunda Hospital has made or plan to make changes to improve the quality of services.
The most recent changes or planned changes are:
Listening to our patients, their families and their carers is one of the most important aspects of delivering high quality care.
Feedback from our patients helps to guide our decision making, and enable us to make changes and improvements to our services. Our patients should feel confident when visiting our hospitals and health services, knowing that their care and experience is our highest priority.
Measuring patient experience
Net Promoter Score
Net Promoter Score (NPS) is used to measure patient experience in our hospitals. The NPS is the percentage of patients who rate their likelihood to recommend our service to a friend or colleague as 9 or 10 ("promoters") minus the percentage who rate 6 or below ("detractors") on a scale from 0 to 10. Patients who provide a score of 7 or 8 are referred to as “passives” and are included the total number of respondents, thus decreasing the percentage of detractors and promoters and have the effect of pushing the score toward 0.
How do we measure up
The graph below shows the Net Promoter Scores for Kalamunda Hospital.
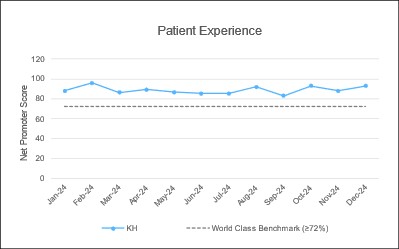
What the figures mean
A Net Promoter Score of higher than 72% is considered World Class and EMHS use this as the benchmark. A higher Net Promoter Score is desirable.
Kalamunda Hospital has performed above benchmark over the past 12 months.

