History and Achievements
Heritage
Bioengineering at Royal Perth Hospital dates back to 1969 when the first engineer was employed by the hospital to provide specialist medical engineering services directly to clinicians. The early emphasis was on the areas of orthopaedics, spinal injuries and rehabilitation. Since that time the service, now known as the Centre for Implant Technology and Retrieval Analysis (CITRA), has developed into a world class facility providing a comprehensive range of bioengineering services to hospitals throughout Western Australia. The key focus for CITRA is in the areas of implant technology, retrieval analysis and in the emerging area of tissue engineering. More than 10,000 devices removed as a routine or due to failure/revision have been subject to investigation and over 1,000 patients during the last 20 years have benefited from specialised custom medical devices; a truly life improving service to Western Australians.
CITRA is a cooperative partnership between engineers, clinicians, scientists, technical staff and researchers. The centre has a focus on innovation and the translation of latest technology into the clinic. This is based on a tradition of excellence in evidence based practice, translational medicine, practical research and teaching.
Clinical Innovation: First Use of Technology
CITRA has a long standing program in custom implant manufacture. Over more than 30 years, many world-firsts have been achieved, some turning into routine clinical services.
2022
Genetic Testing to predict an allergic response to implants used in joint replacement surgery
Some patients who undergo joint replacement surgery develop an allergic response to their artificial implant, increasing their likelihood of repeat surgery and further complications. Our laboratory was part of a ground-breaking international study that identified a genetic marker that predisposes some patients to react badly to cobalt chrome, a material used in most joint implants. As a result of the study, a simple saliva or blood test may soon be available to determine whether a patient falls into this at-risk group.
Arising from the study, an algorithm had been developed that had been shown to predict patient’s risk with a high degree of accuracy. The algorithm combined the presence of the genetic marker with other factors such as the patient’s age and gender (which were associated with risk of hypersensitivity or allergy to cobalt chrome). The study was an international clinical collaboration between our laboratory the UK-based Newcastle University and University Hospital of North Tees and the Hospital for Special Surgery in New York and was published in Nature Communications.
2022
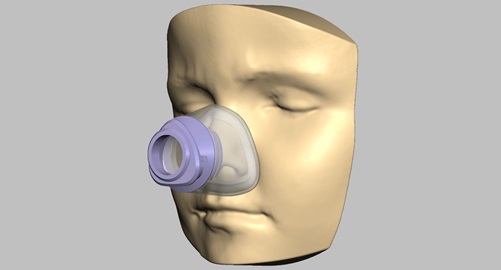
Personalised CPAP masks for paediatric patients
Continuous Positive Airway Pressure (CPAP) devices prevent a user’s windpipe from collapsing during sleep by delivering air – via a tube – into a mask that fits over the user’s nose and mouth. Masks supplied by the machine’s manufacturers, however, may fail to provide a good seal, causing air which should be flowing into the child’s airway, to escape.
This not only deprives the child of oxygen he or she needs during sleep but can also cause painful pressure sores and the escaping air can cause dry eye. The masks can be so uncomfortable that the child will refuse to wear them, increasing their risk of long-term harm.
In collaboration with an Ear, Nose and Throat surgeon at Perth Children’s Hospital, we have developed a mask cushion that is tailored to the face of the individual wearer. While this is particularly important for patients with atypical facial anatomy, it is estimated that about 25 per cent of paediatric patients undergoing CPAP therapy have problems with poor fitting masks.
The process begins with a scan of the child’s face. This takes less than five minutes and can be performed on a hospital ward or at an outpatient appointment. Using 3D printing technology, the scan is used to create a digital replica of the child’s face. This digital replica is used to create a mould for the silicone mask. After proving the custom mash cushion concept on several patients, an approved clinical trial is scheduled to commence in 2023.
2021
Facial contouring following significant trauma
Patients who experience significant facial trauma often require ongoing surgery to achieve a cosmetic outcome to substantially restore their appearance prior to how they looked prior to the trauma. This often includes people involved in motor-vehicle accidents. Achieving an ideal facial contouring post-trauma is a significant challenge, particular for the bones around the eye. We devised a stamp technique to reconstruct a patient’s facial bones, which aided in achieving an ideal facial reconstruction while also saving considerable time in the operating room.
The technique was assess by 3D scanning the patient in the operating room, immediately before and after surgery. This is the world first use of 3D scanning of a patient’s bony structure in surgery.
2021
Custom midface distractor for a 5-year-old child
Midface distraction is a surgical technique to teat patients who require advancement of their facial bones. We were requested to provide a custom-made midface distractor for a 5-year-old patient whose skull was too thin to accommodate the standard midface distractor. Using advanced modelling, prototyping and engineering, we designed a novel distractor which was braced on the back of the patient’s head, where the bone was thicker.
A custom surgical placement guide and a custom cushion was also provided.
2020
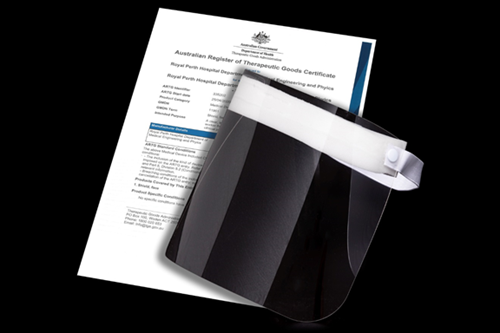
COVID Response – Manufacture and testing of Personal Protective Equipment (PPE)
In response to the COVID pandemic, we established a facility to produce 10,000 face shields. Working closely with university partners, industry partners and Western Australia’s Chief Scientist, we rapidly prototyped and designed a production-line process for producing face shields in large quantities which were approved by the Australian medical regulator, the Therapeutic Goods Administration. This ensured a local supply of this critical PPE at a time when national and international supply lines were disrupted.
We also provided a service for rapidly testing PPE sourced from overseas to determine if it met Australian standards. While we initially used our existing equipment, our capabilities were bolstered by the purchase of dedicated equipment to test face masks, including a Particulate Filtration Efficiency (PFE) Tester and a Synthetic Blood Penetration Resistance tester.
2017
Surgical planning for a 2-day-old baby with an airway blockage (choanal stenosis) requiring life-saving surgery
Solid modelling provides an important additional tool for the planning of complex surgical procedures. Based on CT data, accurate models suitable for use in theatre can be used as an adjunct to imaging.
The clinical innovation of solid modelling pioneered by CITRA is now an important tool for the planning of complex surgical procedures. It's applied through the trial of novel approaches and developments of surgical instruments required to treat complex development cases, like baby Sophia's. It allows surgeons the confidence to perform procedures, and a tactile, visual aid for explaining them to patients and families.
You can read a story about Sophia, who is well and living happily, and watch the Today Tonight story from 2017:
2016
First 3D printed prosthetic ear. Now a routine clinical service for all patients in Western Australia
The potential to manufacture structures using 3D printed polymers or bioprinted facsimiles for use in plastic surgery is regularly canvassed. To overcome problems that exist with current polymers available for rapid prototyping, CITRA has addressed the need, utilising the skills and experience of the maxillofacial technicians using conventional materials and by introducing accurate moulding templates based on surface scanning, CAD and 3D printing. In the early case involving a prosthetic ear, the ear on the contra-lateral side was surface scanned and the shape data was inverted and integrated with the shape of the area to receive the prosthetic ear to produce the final shape to be 3D printed as the pattern for moulding. Successful innovation has been adopted as a routine clinical service to patients in WA and is being adapted for nasal prosthetics. Significant manufacturing efficiency has been achieved.

 First custom stoma plate designed to eliminate leaking in difficult stomas
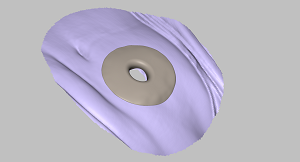
First custom stoma plate designed to eliminate leaking in difficult stomas
The normal difficulties associated with accepting and living with a stoma is exacerbated in difficult cases where leaking occurs; for example, as a result of scarring, adhesions or skin folds in the proximity of the stoma. CITRA provides a routine service to assist with such cases using surface scanning and shape generation techniques from which a custom stoma plate can be manufactured using 3D printing. Currently this requires a pattern to be developed from which a plate can be moulded using conventional polymers and work is in hand to enable the direct manufacture of the plate from the printer.
2015
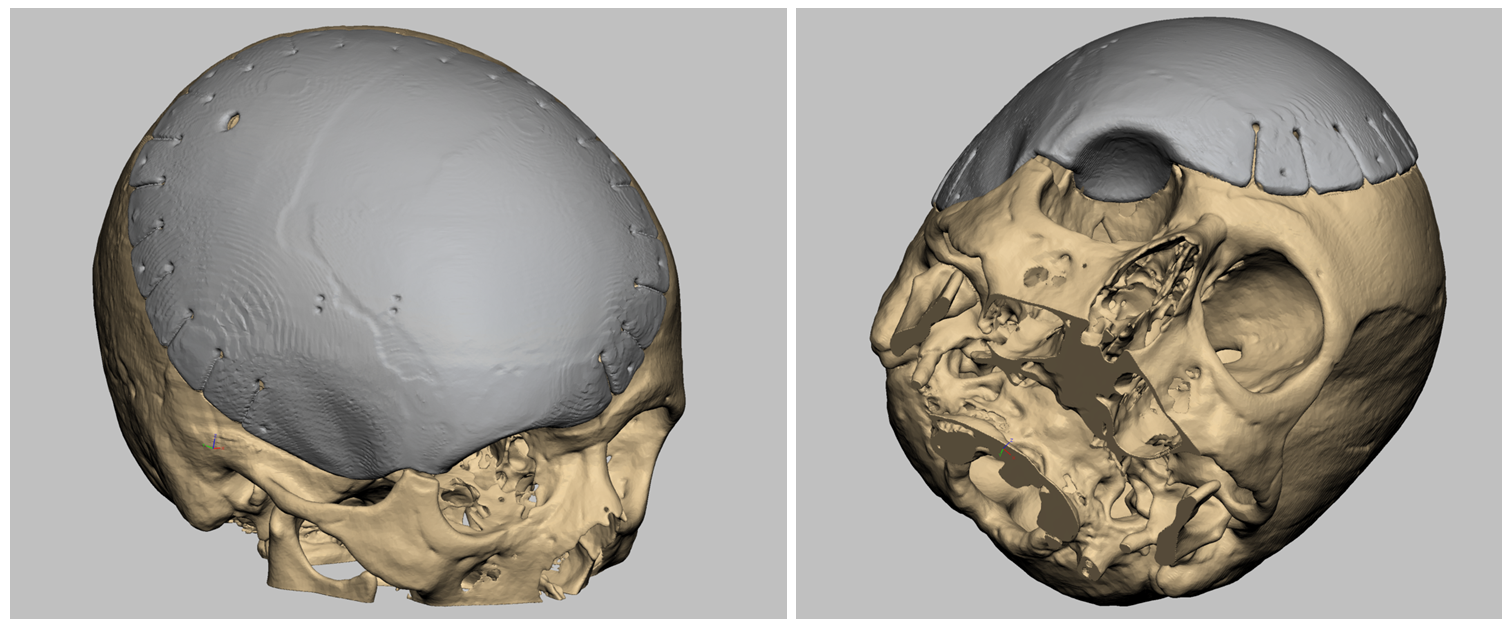
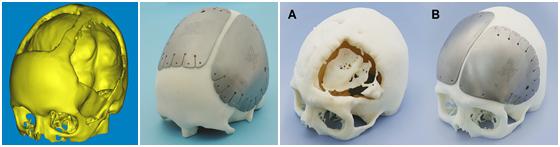
Completion of a double-blind clinical trial in neurosurgery comparing autologous bone to custom-designed titanium implants
In providing custom cranioplasty plates post cranial decompression, the question remains; is it preferable where possible to use the autologous bone removed during the procedure, to close the defect. A study was conducted on 64 patients who had previously been enrolled and randomised to receive either their own bone graft or a primary titanium cranioplasty.
Functional and cosmetic outcomes had previously been assessed at 1-year following the cranioplasty procedure. Hospital records and the Picture Archiving communication system were reviewed to determine how many patients had cranioplasty failure or associated complications such as seizures beyond 1 year – with a minimum of 24-month follow-up. A comparative analysis concluded that bone resorption of the patient allograft continued to occur beyond 12 months after cranioplasty while use of primary titanium cranioplasty after decompressive craniectomy was without significant complication, reducing the number of reoperations needed and the associated long-term total hospital costs. Follow-up at 2 years has indicated increased allograft failure and savings have been estimated at $10k per patient resulting from use the primary use of titanium cranioplasty.
This achievement has been featured on Nine News:
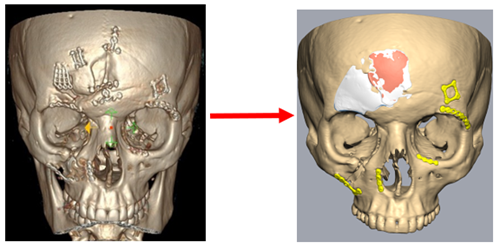
Combined cranio-orbital reconstruction based on a single piece, custom titanium plate and using a 3D printed resection guide
Computer assisted design (CAD) and rapid 3D printing/prototyping technologies provide technology solutions ideally suited to complex surgical reconstruction procedures. This is illustrated by the planned approach taken in a case where substantial resection of cranial bone was required, including partial excision of the orbital socket, in the treatment of a bone cancer. The margin of the excision was determined by the surgeon on the basis of CT information and this data was transferred to the 3D image of the surface on the computer. A template was developed using 3D printing to guide the excision of the cancer affected bone and a custom Ti bone plate, to close the cranial defect including the eye socket was designed and manufactured prior to surgery to match the template to ensure an accurate fit. The multiple objectives of combing excision with accurate reconstruction in a single and definitive procedure, minimising surgical time and reducing potential morbidity while achieving a good cosmetic and medical outcome was achieved.
2014
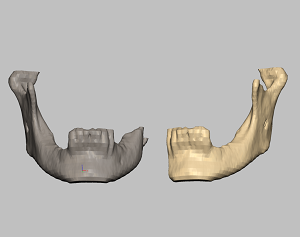 World first case of 3D printing with the patient on the table (mirror mandible reconstruction)
World first case of 3D printing with the patient on the table (mirror mandible reconstruction)
Rapid 3D printing is often cited as having the potential to provide real time solutions required during surgery. This is exemplified in a case conducted at RPH where assistance was requested during reconstructive surgery to provide a template for the adjustment of plates used to fix the sculptured bone grafts replacing approximately half the mandible. Direct access to current CT image data, design experience and onsite printing capacity enabled the construct of a model mirrored to fit the remaining mandible within the surgical timeframe. Ability to sterilise the model enabled its direct use as an accurate template for graft bone and plate adjustment within the surgical field. While planned development is preferred, this case nevertheless demonstrated the capacity to provide expedient and timely assistance if required.
2013
 Australian-first use of custom titanium implants for orbital reconstruction
Australian-first use of custom titanium implants for orbital reconstruction
It is not uncommon in cases of facial trauma from a punch or from impact with the steering wheel or dashboard in road trauma for the eye to incur an orbital blow-out fracture of the medial floor of the cranial socket. Failure to reset the eye can result in an enopthalmous with impaired sight and a poor cosmetic result. Typically a fan plate, hand constructed from Ti mesh during surgery, was available. This method was found to extend surgical times with the need to predict the extent of soft tissue swelling, often resulting in a poor fit.
CITRA, working with the surgeons developed a custom solution for orbital reconstruction offering a range of accurate size options to enhance fitment at the time of surgery. Initial cases involved fractures of long standing resulting in atrophy of the fat pad protecting the eye. The custom device was found to provide a smooth and sympathetic seat for the eye and has developed as the preferred treatment.
First-in-human clinical trial enabling patients to re-grow their own cranial bone in situ from donor stem cells
An alternative to covering a closing a cranial defect using a custom Ti plate is to fill the defect with a porous matrix plate that is populated with donor stem cells. The aim is to support regrowth and integration of the plate with the cranial bone. clinical trial was conducted, subject to scientific scrutiny and ethics approval. The trial was based on a first generation solution using allogenic mesenchymal stromal cells provided by CTTWA, imbedded in a matrix of ceramic granules supported by a polymer mesh. One year follow-up is reported for 3 patients and indicates new bone formation and integration in two cases. Current development is based on porous ceramic plates custom designed to fit the defect and constructed to optimise active cell interaction with the host and the generation of viable bone.
2012
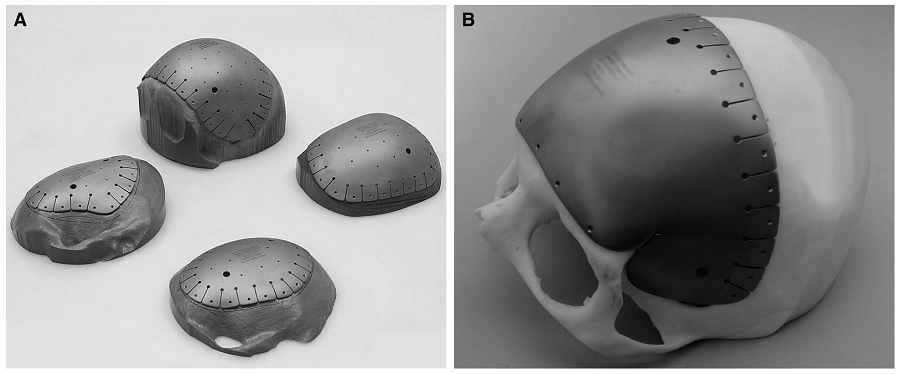
Publication of the largest peer-reviewed case series on cranial reconstruction using custom designed titanium implants
Surgeon involvement and sound scientific and laboratory follow-up provides the clinical based evidence to review an emerging technology. Importantly, the device and the procedure can be assessed, based on sound population data rather than individual case study and anecdote. Publication is encouraged as a means of subjecting innovative practice to a wide ranging peer review.
2010
First double titanium cranioplasty (shortly followed by the second in 2011)
CITRA, working with the TSD Advanced manufacturing facility, has developed a routine methodology for the manufacture of custom cranioplasty plates using 0.6mm surgical grade titanium sheet. The design is based on CT scan data and computer assisted design (CAD) to fit the skull and to mirror the cranial shape. Titanium plating is indicated where the bone removed to allow surgery or brain decompression in trauma cases is extensive and the expected survival of the resected bone after replacement is low. Deep drawing of titanium to fit a mould that is manufactured from the CT data using rapid printing requires a combination of hydrostatic pressing, progressive annealing and hand finishing. Custom plates have been found to provide a secure closure of the skull (protecting the brain), good cosmesis and cost effective surgery.
2006
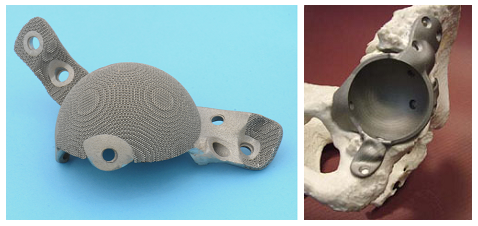
World first use of 3D laser melted (SLM) titanium acetabular reconstruction implants
This device was 3D printed from titanium for a patient who was at risk of losing the ability to walk. This and a number of similar cases, have provided a sound load bearing base to the pelvic acetabulum in cases where the bone stock is depleted. This may result in penetration of the femoral head into the pelvic cavity, particularly under load bearing. The design recognises the need to find a strong attachment to sound bone and is custom manufactured to accept the acetabular cup of the resulting total hip replacement. While this development was based on European technology available at the time, latterly CITRA has been testing and accessing Australian technology.
1997
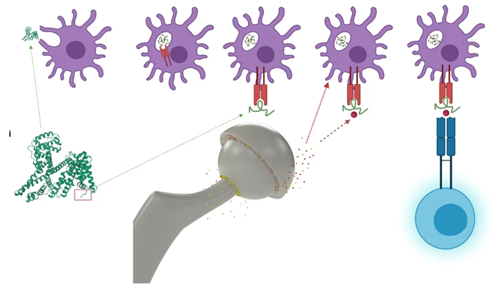
 The RPH Hip Spacer – a device designed and manufactured by CITRA to treat infected joints, allowing the patient to mobilise whilst the infection is treated
The RPH Hip Spacer – a device designed and manufactured by CITRA to treat infected joints, allowing the patient to mobilise whilst the infection is treated
Treatment can be by a combination of systemic administration of antibiotic and the localised exposure of hip joint tissue to the antibiotic delivered by leaching from the femoral head component of the device. In the majority of cases, infection requires removal of the original device. The spacer is inserted to maintain tissue integrity around the joint to allow replacement of the arthroplasty once tissue health is achieved. Stabilisation of the joint using the spacer allows limited ambulation and improves bed rest, enabling the patient to be cared for at home, thus reducing treatment cost. The device is assembled to fit the patient and is available at call, using a kit maintained by CITRA. The RPH Spacer demonstrates the merit of applying engineering practicality to an innovative solution derived from sound clinical insight.
1984
 Manufacture and the early in-human use of a medical device designed on data derived from the patient's CT scan
Manufacture and the early in-human use of a medical device designed on data derived from the patient's CT scan
The object was to retain the use of a functional limb following removal of the upper third of the humerus due to a tumour in a young active male. The imperatives were time and avoidance of a flail arm and/or amputation. Shoulder fixation was achieved using a vascularised bone graft, bridging the scapular and residual humerus and supported by a two part fixation plate manufactured to fit a model of the scapular drafted and built from the CT images. The arthrodesis is still in situ and performing well 30+ years after surgery.