Unplanned Readmissions for Selected Surgical Procedures
‘Readmissions to hospital within 28 days of discharge’ is an indicator of how well we are achieving our objective to provide universal access to services that are coordinated and provide continuity of care.
By measuring and monitoring this indicator, the level of potentially avoidable hospital readmissions can be assessed in order to identify key areas for improvement. This in turn can facilitate the development and delivery of targeted care pathways and interventions, which can help to ensure effective restoration to health and improve the quality of life of Western Australians.
Unplanned and unexpected hospital readmissions within 28 days rates are provided for the following surgical procedures:
- knee replacement,
- hip replacement,
- tonsillectomy & adenoidectomy,
- hysterectomy,
- prostatectomy,
- cataract surgery,
- appendicectomy.
Measuring unplanned readmissions for selected surgical procedures
Readmission rate is considered a global performance measure, as it potentially points to deficiencies in the functioning of the overall healthcare system. Good intervention, appropriate treatment together with good discharge planning will decrease the likelihood of unplanned hospital readmissions. A low unplanned readmission rate suggests that good clinical practice is in operation. These readmissions necessitate patients spending additional periods of time in hospital as well as utilising additional hospital resources.
These indicators are an aggregate result for all EMHS hospitals. Note: Not all surgical procedures are performed at all hospitals.
The benchmark in each of the following categories is based on the best state-wide result within the five calendar years from 2016 - 2020.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart a: Unplanned readmissions of patient discharged following management of knee replacement
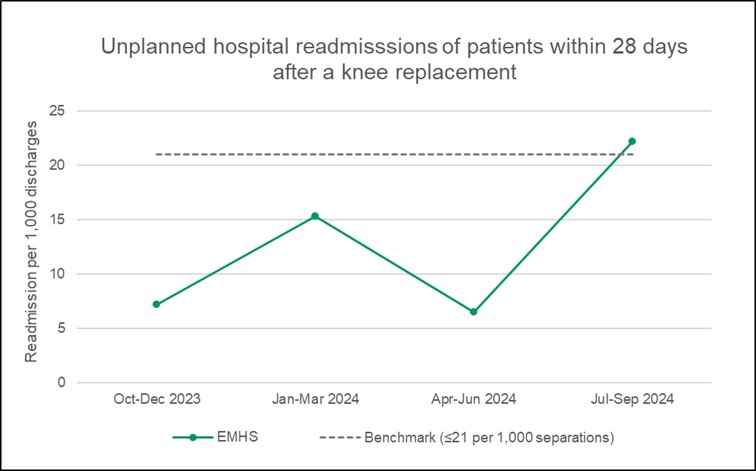
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had a knee replacement. The benchmark is less than or equal to 21 readmissions for every 1,000 discharges, or about 1 re-admission in 47 knee replacements. A rate lower than the benchmark is desirable. The overall rates for EMHS hospitals were lower than the benchmark in three of the last four quarters. While these results represent very small case numbers, several quality improvement actions have been identified from individual case reviews.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart b: Unplanned readmissions of patient discharged following management of hip replacement
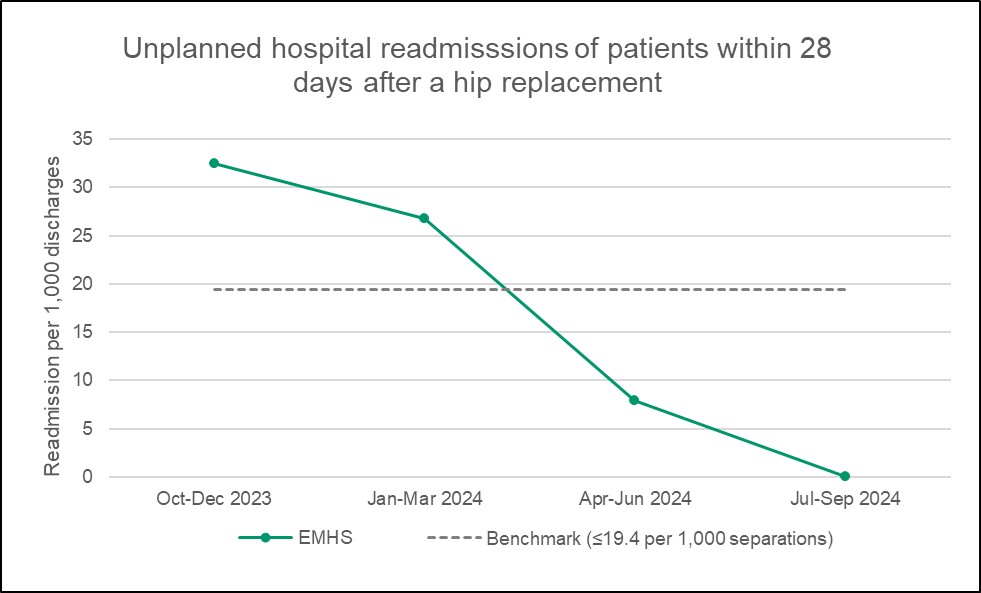
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had a hip replacement. The benchmark is less than or equal to 19.4 readmissions for every 1,000 discharges, or about 1 re-admission in 52 hip replacements. A rate lower than the benchmark is desirable. The overall rates for EMHS hospitals were lower than the benchmark in two of the last four quarters. While these results represent very small case numbers, several quality improvement actions have been identified from individual case reviews.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Bentley Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart c: Unplanned readmissions of patient discharged following management of tonsillectomy and adenoidectomy.
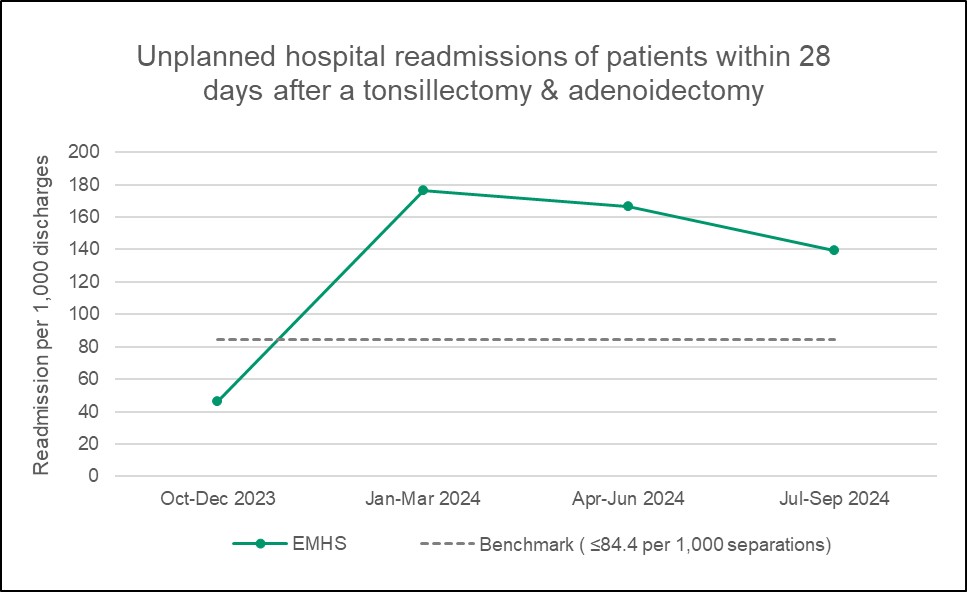
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had a tonsillectomy or adenoidectomy. The benchmark is less than or equal to 84.4 readmissions for every 1,000 discharges, or about 1 re-admission in 12 tonsillectomy/adenoidectomy. A rate lower than the benchmark is desirable. EMHS results have been above the benchmark in three out of the last four quarters. Peer review of all readmissions is conducted as part of the ear, nose and throat (ENT) morbidity and mortality review process and case review has demonstrated that patients are often managed conservatively, being readmitted as a precaution with minor post-operative bleeding.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Bentley Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart d: Unplanned readmissions of patient discharged following management of hysterectomy.
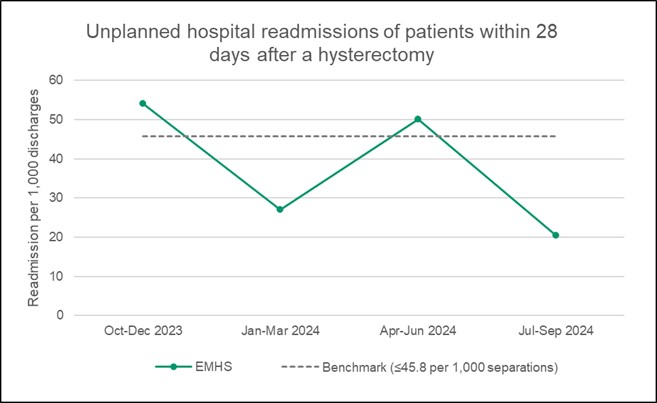
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had a hysterectomy. The benchmark is less than or equal to 45.8 readmissions for every 1,000 discharges, or about 1 re-admission in 22 hysterectomies. A rate lower than the benchmark is desirable. EMHS results have been lower than the benchmark in two of the last four quarters. While these results represent very small case numbers, several quality improvement actions have been identified from individual case reviews.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Bentley Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart e: Unplanned readmissions of patient discharged following management of prostatectomy.
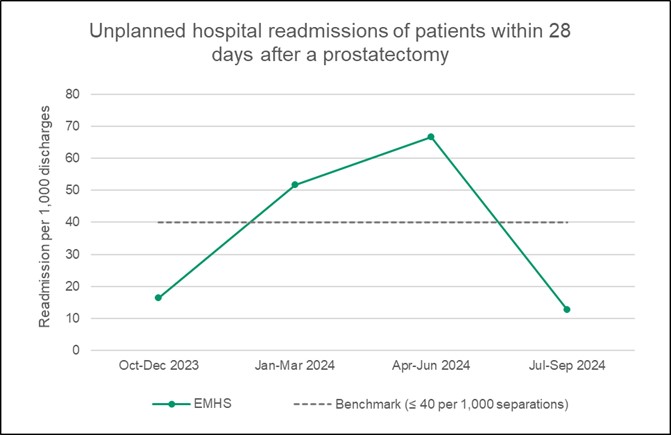
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had a prostatectomy. The benchmark is less than or equal to 40 readmissions for every 1,000 discharges, or about 1 re-admission in 25 prostatectomies. A rate lower than the benchmark is desirable. EMHS results have been lower than the benchmark in two of the last four quarters. While these results represent very small case numbers, several quality improvement actions have been identified from individual case reviews.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Bentley Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart f: Unplanned readmissions of patient discharged following management of cataract surgery
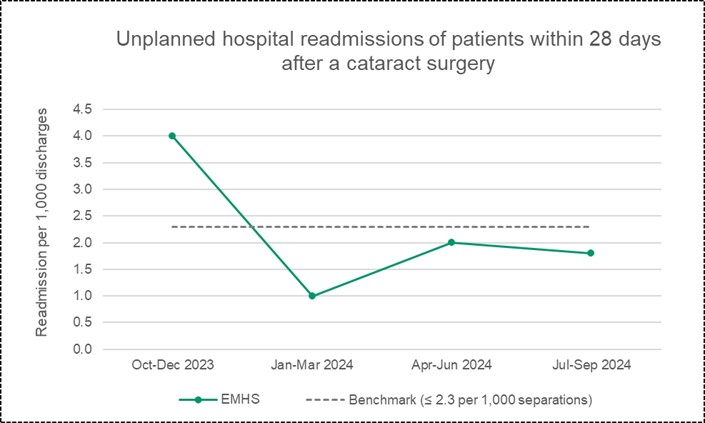
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had cataract surgery.
The benchmark is less than or equal to 2.3 readmissions for every 1,000 discharges, or about 1 re-admission in 435 cataract surgeries. A rate lower than the benchmark is desirable.
EMHS results have been lower than the benchmark in three of the last four quarters. While these results represent very small case numbers, several quality improvement actions have been identified from individual case reviews.
How do we measure up
The graph below shows the unplanned readmissions for selected surgical procedures rate across EMHS hospitals:
- Armadale Health Service
- Royal Perth Hospital
- St John of God Midland Public Hospital
Chart g: Unplanned readmissions of patient discharged following management of appendicectomy.
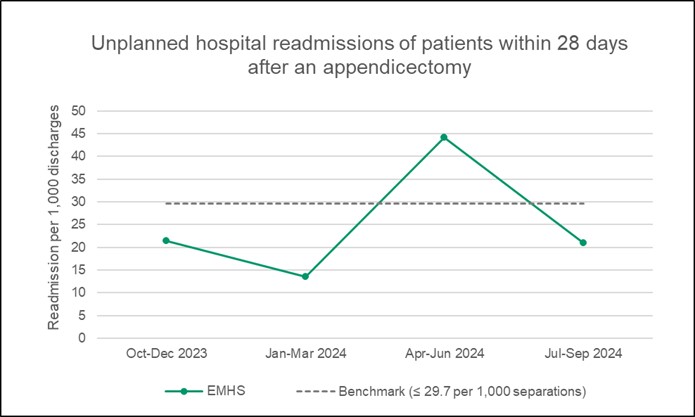
What the figures mean
This indicator counts the number of times patients have needed re-admission to hospital within 28 days of discharge after having had appendicectomies. The benchmark is less than or equal to 29.7 readmissions for every 1,000 discharges, or about 1 re-admission in 34 appendicectomies. A rate lower than the benchmark is desirable. EMHS results have been below the benchmark in three out of the last four quarters. All cases are reviewed by EMHS hospitals to identify common factors that can be addressed to minimise future unplanned readmissions.

