Healthcare-associated Staphylococcus Bloodstream Infections
Infections people get while being cared for in a healthcare facility are known as healthcare associated infections (HAI).
The most common types of infection acquired in hospitals are:
- bloodstream infection
- urinary tract infection (UTI)
- pneumonia (lung infection)
- wound infection.
For a patient, a HAI can result in:
- illness
- an extended stay in hospital
- a slower recovery
- increased stress
- lower morale.
HAIs are costly to patients, hospitals and the community. While they can occur in any healthcare setting, effective infection prevention and control can significantly reduce the infection rate. Patients, visitors and staff all play a role in reducing HAIs.
About Staphylococcus aureus bloodstream infections (SABSIs)
An important cause of common HAI is Staphylococcus aureus (S. aureus), also known as ‘Golden Staph’. It is a type of bacteria often found on the skin of healthy people and is usually harmless. In hospitals, transmission is most commonly via the hands of healthcare workers.
Most cases can be treated by antibiotics; however, there are more serious antibiotic-resistant strains. It is estimated that contracting a healthcare-associated S. aureus bloodstream infection whilst in hospital, can be life-threatening or cause serious harm in 20 to 35 per cent of cases.
Measuring hospital acquired bacteraemia
The rate of healthcare associated S. aureus bloodstream infections (SABSIs) is measured by counting the number of infections and dividing by the number of beds occupied by patients each day (occupied bed days) over a three-month period. For an infection to be considered healthcare-associated there must be no evidence that it was present or developing at the time of hospital admission.
The definition of a SABSI was developed by the Australian Commission on Safety and Quality in Health Care.
The nationally agreed benchmark set under the National Healthcare Agreement (NHA) is no more than 2.0 cases of healthcare associated S. aureus bloodstream infection per 10,000 days of patient care for public hospitals in each state and territory.
WA Health has set a benchmark of less than or equal to 1.0 healthcare associated S. aureus bloodstream infection per 10,000 bed days.
To minimise the risk of patients getting a preventable infection, each EMHS hospital has a surveillance program through which they closely monitor infection rates and evaluate the effectiveness of strategies used to prevent and control SABSIs. Surveillance data is reported throughout all levels of the health service to support good decision-making in the prevention of SABSIs.
All identified cases of infection undergo review by infection control specialists to ascertain anything that the service could have done to prevent the infection. Given the complexity of health care and patients seen, not all cases of infection will be considered preventable.
How do we measure up
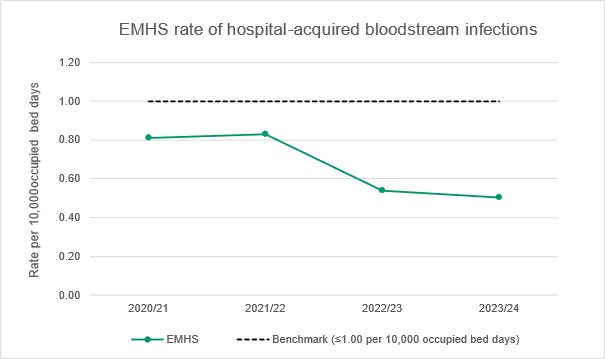
The graph below shows the combined healthcare associated bacteraemia rate for the EMHS hospitals:
- Armadale Health Service
- Kalamunda Hospital
- Bentley Hospital
- Royal Perth Hospital
Chart: Healthcare-associated S. aureus bloodstream infection rate per 10,000 bed days.
What the figures mean
The graph shows the overall rate of S. aureus bloodstream infection across EMHS by financial year.
The benchmark is less than or equal to 1.0 hospital-acquired bloodstream infection per 10,000 occupied bed days. A rate lower than the benchmark is desirable.
The overall rate of S. aureus bloodstream infections across EMHS public hospitals has been consistently below the benchmark. EMHS continues to monitor, review and identify strategies towards prevention of infection.

