RPBG patients benefiting from new at home treatment
Immunoglobulin (Ig) therapy is used to treat patients who are deficient in immunoglobulins (antibodies), which are a vital part of the body’s defence against foreign invaders like bacteria, or viruses.
Patients who have specific haematology, neurology or immunology-based conditions are often required to participate in time consuming treatments at RPH every three to four weeks.
The Ig treatment can typically take anywhere between three and eight hours to administer, resulting in the patient attending the hospital for extended periods of time.
However, for the past nine months, the Standard 7 Blood Management Committee have been working on the development of a self-administered Subcutaneous Immunoglobulin (SCIg) treatment, which could see patients administer the treatment from the comfort of their own home, offering greater freedom and flexibility around when and where they receive their treatment.
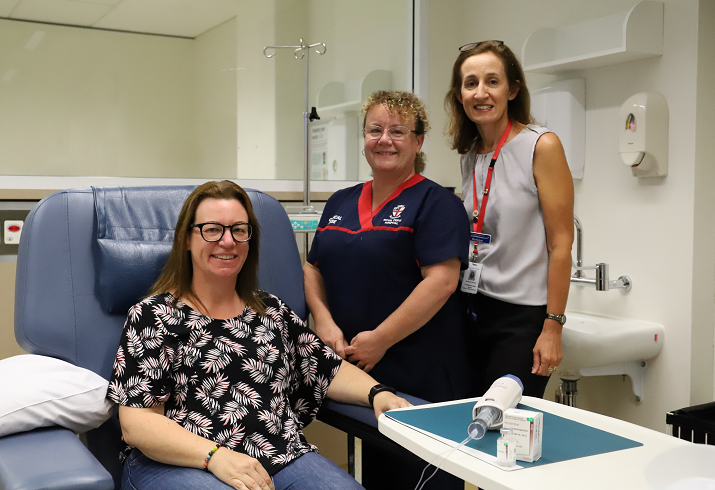
Paula (pictured), who has a neurology condition called Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) which can cause weakness, sensory loss, imbalance and pain which can ultimately lead to substantial disability is the first patient to take part in the self-administering SCIg treatment at Royal Perth Hospital and feels confident in the training she has received by staff throughout the process which allows her to feel comfortable about performing the treatment herself.
“Staff are required to work with the patient to increase the patient’s knowledge base and confidence when it comes to developing new skills to self-administer the treatment.” said project lead Monique Craven. “Overall, the nurses are there to support the patient on this journey and ensure the patient is competent, safe and supported at all times.”
The medication which contains human immunoglobulins, can be used as an antibody replacement when there is a condition that causes an imbalance in your immune system, with the primary goal for CIDP patients like Paula to reduce the symptoms, gain symptom control, and ideally maintain long-term remission.
Patient Paula who has completed her final training with the SCIg nurses, has spent the past two weeks learning about how to store the medication, how to draw the medication up into the pump, how and where to insert the needle, how to deal with a reaction, and how to complete the documentation for each treatment.
“The ability for patients to self-administer allows them to have more time for themselves, with patients now capable of travelling and holidaying without needing to schedule that time around their hospital appointments.”
Patients who take part in this treatment will continue to remain in direct communication with the SCIg nurse, Caran Danskin, and are contacted weekly once administering at home, so staff can review the infusions assess and troubleshoot any issues and allow the patient to liaise with medical staff as required.

